EasySep™ Human NK Cell Isolation Kit
8-Minute cell isolation kit using immunomagnetic negative selection
概要
The EasySep™ Human NK Cell Isolation Kit is designed to isolate NK cells from fresh or previously frozen peripheral blood mononuclear cells or washed leukapheresis samples by immunomagnetic negative selection. The EasySep™ procedure involves labeling unwanted cells with antibody complexes and magnetic particles. The magnetically labeled cells are separated from the untouched desired cells by using an EasySep™ magnet and simply pouring or pipetting the desired cells into a new tube. This product can be used in place of the EasySep™ Human NK Cell Enrichment Kit (Catalog #19055) for even faster cell isolations.
Advantages
• Fast, easy-to-use and column-free
• Up to 94% purity with high recovery
• Isolated cells are untouched
• Up to 94% purity with high recovery
• Isolated cells are untouched
Components
- EasySep™ Human NK Cell Isolation Kit (Catalog #17955)
- EasySep™ Human NK Cell Isolation Cocktail, 1 mL
- EasySep™ Dextran RapidSpheres™, 1 mL
- RoboSep™ Human NK Cell Isolation Kit (Catalog #17955RF)
- EasySep™ Human NK Cell Isolation Cocktail, 1 mL
- EasySep™ Dextran RapidSpheres™, 1 mL
- RoboSep™ Buffer (Catalog #20104)
- RoboSep™ Filter Tips (Catalog #20125)
Magnet Compatibility
• EasySep™ Magnet (Catalog #18000)
• “The Big Easy” EasySep™ Magnet (Catalog #18001)
• Easy 50 EasySep™ Magnet (Catalog #18002)
• EasyEights™ EasySep™ Magnet (Catalog #18103)
• RoboSep™-S (Catalog #21000)
Subtype
Cell Isolation Kits
Cell Type
NK Cells
Species
Human
Sample Source
Leukapheresis, PBMC
Selection Method
Negative
Application
Cell Isolation
Brand
EasySep, RoboSep
Area of Interest
Chimerism, Immunology
技术资料
| Document Type | 产品名称 | Catalog # | Lot # | 语言 |
|---|---|---|---|---|
| Product Information Sheet | EasySep™ Human NK Cell Isolation Kit | 17955 | All | English |
| Product Information Sheet | RoboSep™ Human NK Cell Isolation Kit | 17955RF | All | English |
| Safety Data Sheet 1 | EasySep™ Human NK Cell Isolation Kit | 17955 | All | English |
| Safety Data Sheet 2 | EasySep™ Human NK Cell Isolation Kit | 17955 | All | English |
| Safety Data Sheet 1 | RoboSep™ Human NK Cell Isolation Kit | 17955RF | All | English |
| Safety Data Sheet 2 | RoboSep™ Human NK Cell Isolation Kit | 17955RF | All | English |
数据及文献
Data
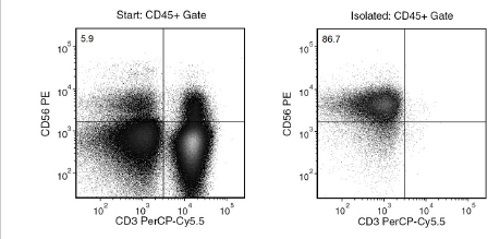
Figure 1. Typical EasySep™ Human NK Cell Isolation Profile
Starting with human PBMCs, the NK cell (CD3-CD56+) content of the isolated fraction is typically 85.0 ± 8.0% (mean ± SD). In the above example, the final purities of the start and isolated fractions are 5.9% and 86.7%, respectively.
Publications (7)
Clinical cancer research : an official journal of the American Association for Cancer Research 2020 jul
Phase II Study of Ensituximab, a Novel Chimeric Monoclonal Antibody, in Adults with Unresectable, Metastatic Colorectal Cancer.
Abstract
Abstract
PURPOSE Patients with metastatic colorectal cancer refractory to chemotherapy have limited treatment options. Ensituximab (NEO-102) is a novel chimeric mAb targeting a variant of MUC5AC with specificity to colorectal cancer. PATIENTS AND METHODS Single-arm, phase II trial assessed the efficacy and safety of ensituximab in patients with advanced, refractory cancer who expressed MUC5AC antigen in tumor tissue. Ensituximab was administered intravenously every 2 weeks with 3 mg/kg as recommended phase II dose (RP2D). A minimum sample size of 43 patients was required on the basis of the assumption that ensituximab would improve median overall survival (OS) by 7 months using a one-sided significance level of 10{\%} and 80{\%} power. Written informed consent was obtained from all patients. RESULTS Sixty-three patients with advanced, refractory colorectal cancer were enrolled and 53 subjects were treated in phase II arm. Median age was 58 years and 46{\%} of the patients were female. Among 57 evaluable patients, median OS was 6.8 months. No responses were observed, and stable disease was achieved in 21{\%} of the patients. The most common treatment-related adverse events (AE) at RP2D included fatigue (38{\%}), anemia (30{\%}), nausea (15{\%}), vomiting (11{\%}), increased bilirubin (9{\%}), constipation (8{\%}), decreased appetite (6{\%}), and diarrhea (6{\%}). Serious AEs at least possibly related to ensituximab occurred in 4 patients and included anemia, nausea, increased bilirubin, and hypoxia. No patients discontinued treatment due to drug-related AEs. CONCLUSIONS Ensituximab was well tolerated and demonstrated modest antitumor activity in patients with heavily pretreated refractory colorectal cancer.
Frontiers in oncology 2020
Evaluation of the Anti-Tumor Activity of the Humanized Monoclonal Antibody NEO-201 in Preclinical Models of Ovarian Cancer.
Abstract
Abstract
Purpose: Despite high initial response rates with cytoreductive surgery, conventional chemotherapy and the incorporation of biologic agents, ovarian cancer patients often relapse and die from their disease. New approaches are needed to improve patient outcomes. This study was designed to evaluate the antitumor activity of NEO-201 monoclonal antibody (mAb) in preclinical models of ovarian cancer where the NEO-201 target is highly expressed. Experimental Design: Functional analysis of NEO-201 against tumor cell lines was performed by antibody-dependent cellular cytotoxicity (ADCC) assays. Binding of NEO-201 to tumor tissues and cell lines were determined by immunohistochemistry (IHC) and flow cytometry, respectively. Further characterization of the antigen recognized by NEO-201 was performed by mass spectrometry. Ovarian cancer models were used to evaluate the anti-tumor activity of NEO-201 in vivo. NEO-201 at a concentration of 250 g/mouse was injected intraperitoneally (IP) on days 1, 4, and 8. Human PBMCs were injected IP simultaneously as effector cells. Results: Both IHC and flow cytometry revealed that NEO-201 binds prominently to the colon, pancreatic, and mucinous ovarian cancer tissues and cell lines. Immunoprecipitation of the antigen recognized by NEO-201 was performed in human ovarian, colon, and pancreatic cancer cell lines. From these screening, carcinoembryonic antigen-related cell adhesion molecule 5 (CEACAM5) and CEACAM6 were identified as the most likely targets of NEO-201. Our results confirmed that NEO-201 binds different types of cancers; the binding is highly selective for the tumor cells without cross reactivity with the surrounding healthy tissue. Functional analysis revealed that NEO-201 mediates ADCC killing against human ovarian and colorectal carcinoma cell lines in vitro. In addition, NEO-201 inhibited tumor growth in the presence of activated human PBMCs in orthotopic mouse models of both primary and metastatic ovarian cancer. Importantly, NEO-201 prolonged survival of tumor-bearing mice. Conclusions: These data suggested that NEO-201 has an antitumor activity against tumor cells expressing its antigen. Targeting an antigen expressed in tumors, but not in normal tissues, allows patient selection for optimal treatment. These findings strongly indicate that NEO-201 warrants clinical testing as both a novel therapeutic and diagnostic agent for treatment of ovarian carcinomas. A first in human clinical trial evaluating NEO-201 in adults with chemo-resistant solid tumors is ongoing at the NIH clinical Center.
Cell reports 2019 nov
Latency-Reversing Agents Induce Differential Responses in Distinct Memory CD4 T Cell Subsets in Individuals on Antiretroviral Therapy.
Abstract
Abstract
Latent proviruses persist in central (TCM), transitional (TTM), and effector (TEM) memory cells. We measured the levels of cellular factors involved in HIV gene expression in these subsets. The highest levels of acetylated H4, active nuclear factor $\kappa$B (NF-$\kappa$B), and active positive transcription elongation factor b (P-TEFb) were measured in TEM, TCM, and TTM cells, respectively. Vorinostat and romidepsin display opposite abilities to induce H4 acetylation across subsets. Protein kinase C (PKC) agonists are more efficient at inducing NF-$\kappa$B phosphorylation in TCM cells but more potent at activating PTEF-b in the TEM subset. We selected the most efficient latency-reversing agents (LRAs) and measured their ability to reverse latency in each subset. While ingenol alone has modest activities in the three subsets, its combination with a histone deacetylase inhibitor (HDACi) dramatically increases latency reversal in TCM cells. Altogether, these results indicate that cellular HIV reservoirs are differentially responsive to common LRAs and suggest that combination of compounds will be required to achieve latency reversal in all subsets.
JCI insight 2019 apr
Identification of rare HIV-1-infected patients with extreme CD4+ T cell decline despite ART-mediated viral suppression.
Abstract
Abstract
BACKGROUND The goal of antiretroviral therapy (ART) is to suppress HIV-1 replication and reconstitute CD4+ T cells. Here, we report on HIV-infected individuals who had a paradoxical decline in CD4+ T cells despite ART-mediated suppression of plasma HIV-1 load (pVL). We defined such an immunological outcome as extreme immune decline (EXID). METHODS EXID's clinical and immunological characteristics were compared to immunological responders (IRs), immunological nonresponders (INRs), healthy controls (HCs), and idiopathic CD4+ lymphopenia (ICL) patients. T cell immunophenotyping and assembly/activation of inflammasomes were evaluated by flow cytometry. PBMC transcriptome analysis and genetic screening for pathogenic variants were performed. Levels of cytokines/chemokines were measured by electrochemiluminescence. Luciferase immunoprecipitation system and NK-mediated antibody-dependent cellular cytotoxicity (ADCC) assays were used to identify anti-lymphocyte autoantibodies. RESULTS EXIDs were infected with non-B HIV-1 subtypes and after 192 weeks of consistent ART-mediated pVL suppression had a median CD4+ decrease of 157 cells/mul, compared with CD4+ increases of 193 cells/mul and 427 cells/mul in INR and IR, respectively. EXID had reduced naive CD4+ T cells, but similar proportions of cycling CD4+ T cells and HLA-DR+CD38+CD8+ T cells compared with IR and INR. Levels of inflammatory cytokines were also similar in EXID and INR, but the IL-7 axis was profoundly perturbed compared with HC, IR, INR, and ICL. Genes involved in T cell and monocyte/macrophage function, autophagy, and cell migration were differentially expressed in EXID. Two of the 5 EXIDs had autoantibodies causing ADCC, while 2 different EXIDs had an increased inflammasome/caspase-1 activation despite consistently ART-suppressed pVL. CONCLUSIONS EXID is a distinct immunological outcome compared with previously described INR. Anti-CD4+ T cell autoantibodies and aberrant inflammasome/caspase-1 activation despite suppressed HIV-1 viremia are among the mechanisms responsible for EXID.
Nature communications 2018 NOV
Human antibodies targeting Zika virus NS1 provide protection against disease in a mouse model.
Abstract
Abstract
Zika virus is a mosquito-borne flavivirus closely related to dengue virus that can cause severe disease in humans, including microcephaly in newborns and Guillain-Barr{\'{e}} syndrome in adults. Specific treatments and vaccines for Zika virus are not currently available. Here, we isolate and characterize four monoclonal antibodies (mAbs) from an infected patient that target the non-structural protein NS1. We show that while these antibodies are non-neutralizing, NS1-specific mAbs can engage Fc$\gamma$R without inducing antibody dependent enhancement (ADE) of infection in vitro. Moreover, we demonstrate that mAb AA12 has protective efficacy against lethal challenges of African and Asian lineage strains of Zika virus in Stat2-/- mice. Protection is Fc-dependent, as a mutated antibody unable to activate known Fc effector functions or complement is not protective in vivo. This study highlights the importance of the ZIKV NS1 protein as a potential vaccine antigen.
The Journal of clinical investigation 2018 JUN
Dose intensification of TRAIL-inducing ONC201 inhibits metastasis and promotes intratumoral NK cell recruitment.
Abstract
Abstract
ONC201 is a first-in-class, orally active antitumor agent that upregulates cytotoxic TRAIL pathway signaling in cancer cells. ONC201 has demonstrated safety and preliminary efficacy in a first-in-human trial in which patients were dosed every 3 weeks. We hypothesized that dose intensification of ONC201 may impact antitumor efficacy. We discovered that ONC201 exerts dose- and schedule-dependent effects on tumor progression and cell death signaling in vivo. With dose intensification, we note a potent anti-metastasis effect and inhibition of cancer cell migration and invasion. Our preclinical results prompted a change in ONC201 dosing in all open clinical trials. We observed accumulation of activated NK+ and CD3+ cells within ONC201-treated tumors and that NK cell depletion inhibits ONC201 efficacy in vivo, including against TRAIL/ONC201-resistant Bax-/- tumors. Immunocompetent NCR1-GFP mice, in which NK cells express GFP, demonstrated GFP+ NK cell infiltration of syngeneic MC38 colorectal tumors. Activation of primary human NK cells and increased degranulation occurred in response to ONC201. Coculture experiments identified a role for TRAIL in human NK-mediated antitumor cytotoxicity. Preclinical results indicate the potential utility for ONC201 plus anti-PD-1 therapy. We observed an increase in activated TRAIL-secreting NK cells in the peripheral blood of patients after ONC201 treatment. The results offer what we believe to be a unique pathway of immune stimulation for cancer therapy.