EasySep™ Mouse CD4+ T Cell Isolation Kit
15-Minute cell isolation kit using immunomagnetic negative selection
概要
The EasySep™ Mouse CD4+ T Cell Isolation Kit is designed to isolate CD4+ T cells from single-cell suspensions of splenocytes or other tissues by negative selection. Unwanted cells are targeted for removal with biotinylated antibodies directed against non-CD4+ T cells and streptavidin-coated magnetic particles (RapidSpheres™ ). Labeled cells are separated using an EasySep™ magnet without the use of columns. Desired cells are poured off into a new tube.
This product replaces the EasySep™ Mouse CD4+ T Cell Enrichment Kit (Catalog #19752) for even faster cell isolations.
This product replaces the EasySep™ Mouse CD4+ T Cell Enrichment Kit (Catalog #19752) for even faster cell isolations.
Advantages
• Fast and easy-to-use
• Up to 96% purity
• No columns required
• Untouched, viable cells
• Up to 96% purity
• No columns required
• Untouched, viable cells
Components
- EasySep™ Mouse CD4+ T Cell Isolation Kit (Catalog #19852)
- EasySep™ Mouse CD4+ T Cell Isolation Cocktail, 0.5 mL
- EasySep™ Streptavidin RapidSpheres™ 50001, 1 mL
- Normal Rat Serum, 2 mL
- RoboSep™ Mouse CD4+ T Cell Isolation Kit (Catalog #19852RF)
- EasySep™ Mouse CD4+ T Cell Isolation Cocktail, 0.5 mL
- EasySep™ Streptavidin RapidSpheres™ 50001, 1 mL
- Normal Rat Serum, 2 mL
- RoboSep™ Buffer (Catalog #20104)
- RoboSep™ Filter Tips (Catalog #20125)
Magnet Compatibility
• EasySep™ Magnet (Catalog #18000)
• “The Big Easy” EasySep™ Magnet (Catalog #18001)
• EasyEights™ EasySep™ Magnet (Catalog #18103)
• RoboSep™-S (Catalog #21000)
Subtype
Cell Isolation Kits
Cell Type
T Cells, T Cells, CD4+
Species
Mouse
Sample Source
Other, Spleen
Selection Method
Negative
Application
Cell Isolation
Brand
EasySep, RoboSep
Area of Interest
Immunology
技术资料
| Document Type | 产品名称 | Catalog # | Lot # | 语言 |
|---|---|---|---|---|
| Product Information Sheet | EasySep™ Mouse CD4+ T Cell Isolation Kit | 19852 | All | English |
| Product Information Sheet | RoboSep™ Mouse CD4+ T Cell Isolation Kit | 19852RF | All | English |
| Safety Data Sheet 1 | EasySep™ Mouse CD4+ T Cell Isolation Kit | 19852 | All | English |
| Safety Data Sheet 2 | EasySep™ Mouse CD4+ T Cell Isolation Kit | 19852 | All | English |
| Safety Data Sheet 3 | EasySep™ Mouse CD4+ T Cell Isolation Kit | 19852 | All | English |
| Safety Data Sheet 1 | RoboSep™ Mouse CD4+ T Cell Isolation Kit | 19852RF | All | English |
| Safety Data Sheet 2 | RoboSep™ Mouse CD4+ T Cell Isolation Kit | 19852RF | All | English |
| Safety Data Sheet 3 | RoboSep™ Mouse CD4+ T Cell Isolation Kit | 19852RF | All | English |
数据及文献
Data
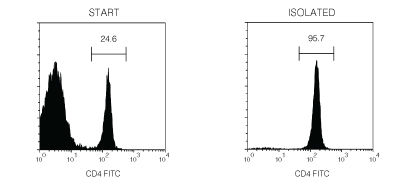
Figure 1. Typical EasySep™ Mouse CD4+ T Cell Isolation Profile
Starting with mouse splenocytes, the CD4+ T cell content of the isolated fraction typically ranges from 89 - 96%.
Publications (26)
Nature biomedical engineering 2020 oct
Prolonged residence of an albumin-IL-4 fusion protein in secondary lymphoid organs ameliorates experimental autoimmune encephalomyelitis.
Abstract
Abstract
Interleukin-4 (IL-4) suppresses the development of multiple sclerosis in a murine model of experimental autoimmune encephalomyelitis (EAE). Here, we show that, in mice with EAE, the accumulation and persistence in the lymph nodes and spleen of a systemically administered serum albumin (SA)-IL-4 fusion protein leads to higher efficacy in preventing disease development than the administration of wild-type IL-4 or of the clinically approved drug fingolimod. We also show that the SA-IL-4 fusion protein prevents immune-cell infiltration in the spinal cord, decreases integrin expression in antigen-specific CD4+ T cells, increases the number of granulocyte-like myeloid-derived suppressor cells (and their expression of programmed-death-ligand-1) in spinal cord-draining lymph nodes and decreases the number of T helper 17 cells, a pathogenic cell population in EAE. In mice with chronic EAE, SA-IL-4 inhibits immune-cell infiltration into the spinal cord and completely abrogates immune responses to myelin antigen in the spleen. The SA-IL-4 fusion protein may be prophylactically and therapeutically advantageous in the treatment of multiple sclerosis.
Science signaling 2020 oct
Modulation of PKM activity affects the differentiation of TH17 cells.
Abstract
Abstract
Small molecules that promote the metabolic activity of the pyruvate kinase isoform PKM2, such as TEPP-46 and DASA-58, limit tumorigenesis and inflammation. To understand how these compounds alter T cell function, we assessed their therapeutic activity in a mouse model of T cell-mediated autoimmunity that mimics multiple sclerosis (MS). TH17 cells are believed to orchestrate MS pathology, in part, through the production of two proinflammatory cytokines: interleukin-17 (IL-17) and GM-CSF. We found that both TEPP-46 and DASA-58 suppressed the development of IL-17-producing TH17 cells but increased the generation of those producing GM-CSF. This switch redirected disease pathology from the spinal cord to the brain. In addition, we found that activation of PKM2 interfered with TGF-$\beta$1 signaling, which is necessary for the development of TH17 and regulatory T cells. Collectively, our data clarify the therapeutic potential of PKM2 activators in MS-like disease and how these agents alter T cell function.
The Journal of experimental medicine 2020 aug
Mechanosensing through YAP controls T cell activation and metabolism.
Abstract
Abstract
Upon immunogenic challenge, lymph nodes become mechanically stiff as immune cells activate and proliferate within their encapsulated environments, and with resolution, they reestablish a soft baseline state. Here we show that sensing these mechanical changes in the microenvironment requires the mechanosensor YAP. YAP is induced upon activation and suppresses metabolic reprogramming of effector T cells. Unlike in other cell types in which YAP promotes proliferation, YAP in T cells suppresses proliferation in a stiffness-dependent manner by directly restricting the translocation of NFAT1 into the nucleus. YAP slows T cell responses in systemic viral infections and retards effector T cells in autoimmune diabetes. Our work reveals a paradigm whereby tissue mechanics fine-tune adaptive immune responses in health and disease.
Nature communications 2020
T cell-intrinsic role for Nod2 in protection against Th17-mediated uveitis.
Abstract
Abstract
Mutations in nucleotide-binding oligomerization domain-containing protein 2 (NOD2) cause Blau syndrome, an inflammatory disorder characterized by uveitis. The antimicrobial functions of Nod2 are well-established, yet the cellular mechanisms by which dysregulated Nod2 causes uveitis remain unknown. Here, we report a non-conventional, T cell-intrinsic function for Nod2 in suppression of Th17 immunity and experimental uveitis. Reconstitution of lymphopenic hosts with Nod2-/- CD4+ T cells or retina-specific autoreactive CD4+ T cells lacking Nod2 reveals a T cell-autonomous, Rip2-independent mechanism for Nod2 in uveitis. In naive animals, Nod2 operates downstream of TCR ligation to suppress activation of memory CD4+ T cells that associate with an autoreactive-like profile involving IL-17 and Ccr7. Interestingly, CD4+ T cells from two Blau syndrome patients show elevated IL-17 and increased CCR7. Our data define Nod2 as a T cell-intrinsic rheostat of Th17 immunity, and open new avenues for T cell-based therapies for Nod2-associated disorders such as Blau syndrome.
Journal of immunology (Baltimore, Md. : 1950) 2019 jul
Nanoparticles Containing an Insulin-ChgA Hybrid Peptide Protect from Transfer of Autoimmune Diabetes by Shifting the Balance between Effector T Cells and Regulatory T Cells.
Abstract
Abstract
CD4 T cells play a critical role in promoting the development of autoimmunity in type 1 diabetes. The diabetogenic CD4 T cell clone BDC-2.5, originally isolated from a NOD mouse, has been widely used to study the contribution of autoreactive CD4 T cells and relevant Ags to autoimmune diabetes. Recent work from our laboratory has shown that the Ag for BDC-2.5 T cells is a hybrid insulin peptide (2.5HIP) consisting of an insulin C-peptide fragment fused to a peptide from chromogranin A (ChgA) and that endogenous 2.5HIP-reactive T cells are major contributors to autoimmune pathology in NOD mice. The objective of this study was to determine if poly(lactide-co-glycolide) (PLG) nanoparticles (NPs) loaded with the 2.5HIP Ag (2.5HIP-coupled PLG NPs) can tolerize BDC-2.5 T cells. Infusion of 2.5HIP-coupled PLG NPs was found to prevent diabetes in an adoptive transfer model by impairing the ability of BDC-2.5 T cells to produce proinflammatory cytokines through induction of anergy, leading to an increase in the ratio of Foxp3+ regulatory T cells to IFN-gamma+ effector T cells. To our knowledge, this work is the first to use a hybrid insulin peptide, or any neoepitope, to re-educate diabetogenic T cells and may have significant implications for the development of an Ag-specific therapy for type 1 diabetes patients.
Scientific reports 2019 apr
Maf deficiency in T cells dysregulates Treg - TH17 balance leading to spontaneous colitis.
Abstract
Abstract
The maintenance of homeostasis in the gut is a major challenge for the immune system. Here we demonstrate that the transcription factor MAF plays a central role in T cells for the prevention of gastro-intestinal inflammation. Conditional knock out mice lacking Maf in all T cells developed spontaneous late-onset colitis, correlating with a decrease of FOXP3+RORgammat+ T cells proportion, dampened IL-10 production in the colon and an increase of inflammatory TH17 cells. Strikingly, FOXP3+ specific conditional knock out mice for MAF did not develop colitis and demonstrated normal levels of IL-10 in their colon, despite the incapacity of regulatory T cells lacking MAF to suppress colon inflammation in Rag1-/- mice transferred with na{\{i}}ve CD4+ T cells. We showed that one of the cellular sources of IL-10 in the colon of these mice are TH17 cells. Thus MAF is critically involved in the maintenance of the gut homeostasis by regulating the balance between Treg and TH17 cells either at the level of their differentiation or through the modulation of their functions."