PneumaCult™-ALI Medium
Serum- and BPE-free medium for human airway epithelial cells cultured at the air-liquid interface
概要
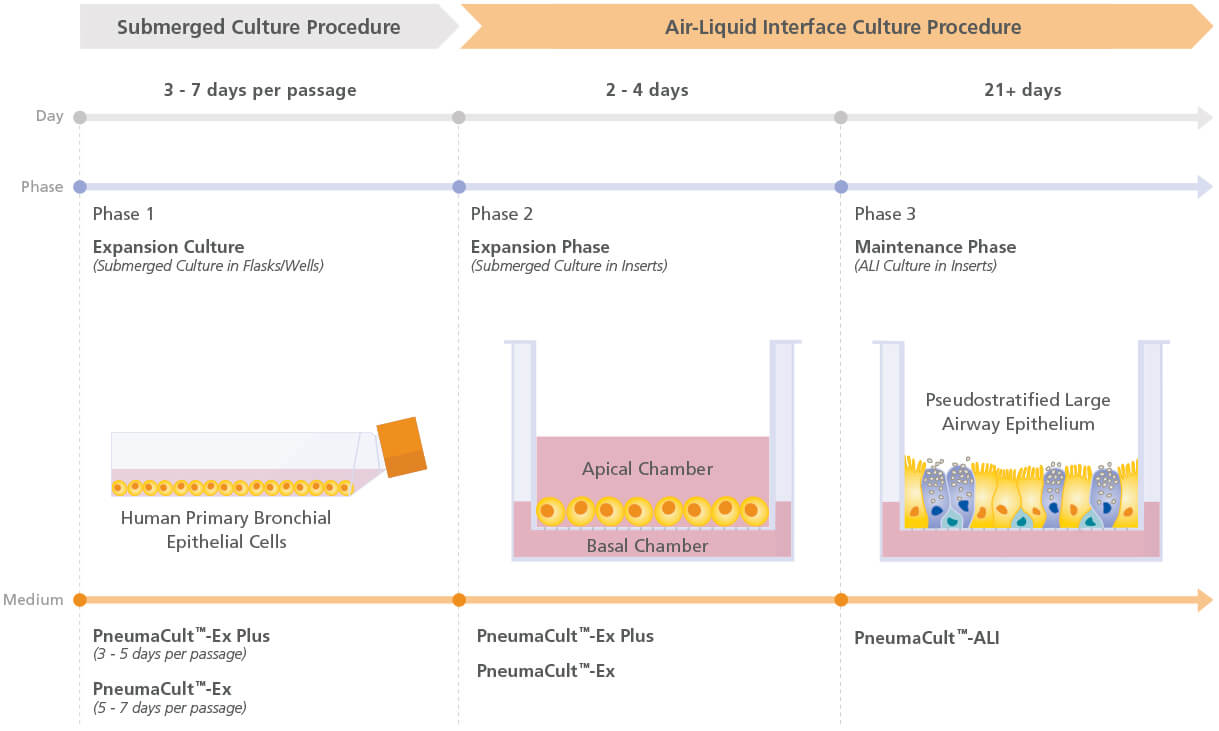
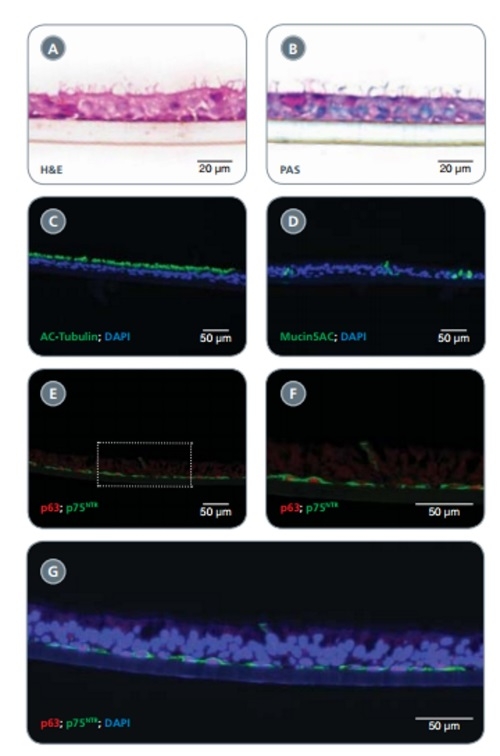
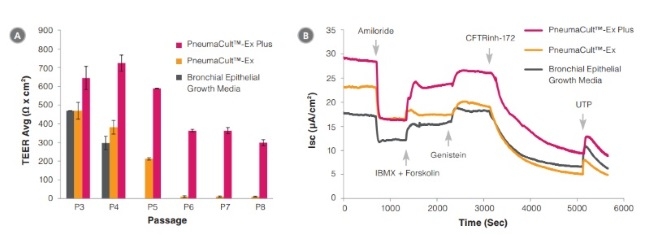
PneumaCult™-ALI Medium (Catalog #05001) is a serum- and BPE-free medium for the culture of human airway epithelial cells at the air-liquid interface (ALI). Airway epithelial cells cultured in PneumaCult™-ALI Medium undergo extensive mucociliary differentiation to form a pseudostratified epithelium that exhibits morphological and functional characteristics similar to those of the human airway in vivo. PneumaCult™-ALI Medium is also available in a kit that includes 12 mm Transwell® inserts (Catalog #05021) or 6.5 mm Transwell® inserts (Catalog #05022).
Together, PneumaCult™-ALI Medium and PneumaCult™-Ex Plus Medium (Catalog #05040) constitute a fully integrated BPE-free culture system for in vitro human airway modeling. This robust and defined system is a valuable tool for basic respiratory research, toxicity studies, and drug development.
• HBECs cultured with PneumaCult™-ALI undergo extensive mucociliary differentiation to form a pseudostratified epithelium that closely resembles the human airway
• PneumaCult™-ALI is serum-free and BPE-free to minimize variability
- PneumaCult™-ALI Basal Medium, 450 mL
- PneumaCult™-ALI 10X Supplement, 50 mL
- PneumaCult™-ALI Maintenance Supplement (100X), 5 x 1 mL
Cell Culture, Differentiation, Maintenance, Organoid Culture
Disease Modeling, Drug Discovery and Toxicity Testing, Epithelial Cell Biology
数据及文献
Publications (98)
Cells 2020 sep
Choice of Differentiation Media Significantly Impacts Cell Lineage and Response to CFTR Modulators in Fully Differentiated Primary Cultures of Cystic Fibrosis Human Airway Epithelial Cells.
V. Saint-Criq et al.
Abstract
In vitro cultures of primary human airway epithelial cells (hAECs) grown at air-liquid interface have become a valuable tool to study airway biology under normal and pathologic conditions, and for drug discovery in lung diseases such as cystic fibrosis (CF). An increasing number of different differentiation media, are now available, making comparison of data between studies difficult. Here, we investigated the impact of two common differentiation media on phenotypic, transcriptomic, and physiological features of CF and non-CF epithelia. Cellular architecture and density were strongly impacted by the choice of medium. RNA-sequencing revealed a shift in airway cell lineage; one medium promoting differentiation into club and goblet cells whilst the other enriched the growth of ionocytes and multiciliated cells. Pathway analysis identified differential expression of genes involved in ion and fluid transport. Physiological assays (intracellular/extracellular pH, Ussing chamber) specifically showed that ATP12A and CFTR function were altered, impacting pH and transepithelial ion transport in CF hAECs. Importantly, the two media differentially affected functional responses to CFTR modulators. We argue that the effect of growth conditions should be appropriately determined depending on the scientific question and that our study can act as a guide for choosing the optimal growth medium for specific applications.
Redox biology 2020 sep
Glutaredoxin deficiency promotes activation of the transforming growth factor beta pathway in airway epithelial cells, in association with fibrotic airway remodeling.
S. B. Chia et al.
Abstract
S-glutathionylation of reactive protein cysteines is a post-translational event that plays a critical role in transducing signals from oxidants into biological responses. S-glutathionylation can be reversed by the deglutathionylating enzyme glutaredoxin (GLRX). We have previously demonstrated that ablation of Glrx sensitizes mice to the development of parenchymal lung fibrosis(1). It remains unclear whether GLRX also controls airway fibrosis, a clinical feature relevant to asthma and chronic obstructive pulmonary disease, and whether GLRX controls the biology of airway epithelial cells, which have been implicated in the pathophysiology of these diseases. In the present study we utilized a house dust mite (HDM) model of allergic airway disease in wild type (WT) and Glrx-/- mice on a C57BL/6 background prone to develop airway fibrosis, and tracheal basal stem cells derived from WT mice, global Glrx-/- mice, or bi-transgenic mice allowing conditional ablation of the Glrx gene. Herein we show that absence of Glrx led to enhanced HDM-induced collagen deposition, elevated levels of transforming growth factor beta 1 (TGFB1) in the bronchoalveolar lavage, and resulted in increases in airway hyperresponsiveness. Airway epithelial cells isolated from Glrx-/- mice or following conditional ablation of Glrx showed spontaneous increases in secretion of TGFB1. Glrx-/- basal cells also showed spontaneous TGFB pathway activation, in association with increased expression of mesenchymal genes, including collagen 1a1 and fibronectin. Overall, these findings suggest that GLRX regulates airway fibrosis via a mechanism(s) that involve the plasticity of basal cells, the stem cells of the airways.
Journal of cystic fibrosis : official journal of the European Cystic Fibrosis Society 2020 sep
Functional rescue of c.3846G\textgreaterA (W1282X) in patient-derived nasal cultures achieved by inhibition of nonsense mediated decay and protein modulators with complementary mechanisms of action.
O. Laselva et al.
Abstract
BACKGROUND The nonsense mutation, c.3846G{\textgreater}A (aka: W1282X-CFTR) leads to a truncated transcript that is susceptible to nonsense-mediated decay (NMD) and produces a shorter protein that is unstable and lacks normal channel activity in patient-derived tissues. However, if overexpressed in a heterologous expression system, the truncated mutant protein has been shown to mediate CFTR channel function following the addition of potentiators. In this study, we asked if a quadruple combination of small molecules that together inhibit nonsense mediated decay, stabilize both halves of the mutant protein and potentiate CFTR channel activity could rescue the functional expression of W1282X-CFTR in patient derived nasal cultures. METHODS We identified the CFTR domains stabilized by corrector compounds supplied from AbbVie using a fragment based, biochemical approach. Rescue of the channel function of W1282X.-CFTR protein by NMD inhibition and small molecule protein modulators was studied using a bronchial cell line engineered to express W1282X and in primary nasal epithelial cultures derived from four patients homozygous for this mutation. RESULTS We confirmed previous studies showing that inhibition of NMD using the inhibitor: SMG1i, led to an increased abundance of the shorter transcript in a bronchial cell line. Interestingly, on top of SMG1i, treatment with a combination of two new correctors developed by Galapagos/AbbVie (AC1 and AC2-2, separately targeting either the first or second half of CFTR and promoting assembly, significantly increased the potentiated channel activity by the mutant in the bronchial epithelial cell line and in patient-derived nasal epithelial cultures. The average rescue effect in primary cultures was approximately 50{\%} of the regulated chloride conductance measured in non-CF cultures. CONCLUSIONS These studies provide the first in-vitro evidence in patient derived airway cultures that the functional defects incurred by W1282X, has the potential to be effectively repaired pharmacologically.
International forum of allergy {\&} rhinology 2020 sep
Interleukin 13 (IL-13) alters hypoxia-associated genes and upregulates CD73.
S. M. Khalil et al.
Abstract
BACKGROUND Interleukin 13 (IL-13) is a pleiotropic cytokine that has been shown to be important in the pathogenesis of chronic rhinosinusitis with nasal polyps (CRSwNP) and other type 2 inflammation-related diseases. Increased IL-13 expression can elicit several pro-inflammatory effects, including eosinophilia, and pathology such as increased mucus secretion. Polypogenesis in chronic rhinosinusitis (CRS) can be caused by hypoxia, which can also lead to hyperpermeability of airway epithelium and epithelium-to-mesenchymal translation through the upregulation of hypoxia-associated genes, such as HIF1. Whether T-helper 2 (Th2) inflammatory cytokines, such as IL-13, can also induce sinonasal epithelial hypoxia-associated genes is currently unknown. METHODS Human air-liquid interface (ALI) sinonasal epithelial cell cultures treated with recombinant IL-13 were analyzed by real-time polymerase chain reaction (PCR) and flow cytometry to determine the effect on epithelial cells. RESULTS Whole tissue from CRSwNP subjects showed increased HIF1A gene expression. Treatment of fully differentiated human ALI cultures with IL-13 resulted in a concurrent increase in HIF1A and ARNT messenger RNA (mRNA) expression. However, the level of EPAS1 expression was significantly reduced. IL-13 also had a dose-dependent response on the expression of HIF genes and the time course experiment showed peak expression of HIF1A and ARNT at 5 to 7 days poststimulation. Remarkably, CD73 surface expression also peaked at day 5 poststimulation. CONCLUSION Our data suggests that IL-13 can induce hypoxia signaling pathway genes leading to surface expression of CD73, which has an anti-inflammatory effect.
Cells 2020 sep
Ionocytes and CFTR Chloride Channel Expression in Normal and Cystic Fibrosis Nasal and Bronchial Epithelial Cells.
P. Scudieri et al.
Abstract
The airway epithelium contains ionocytes, a rare cell type with high expression of Forkhead Box I1 (FOXI1) transcription factor and Cystic Fibrosis Transmembrane conductance Regulator (CFTR), a chloride channel that is defective in cystic fibrosis (CF). Our aim was to verify if ionocyte development is altered in CF and to investigate the relationship between ionocytes and CFTR-dependent chloride secretion. We collected nasal cells by brushing to determine ionocyte abundance. Nasal and bronchial cells were also expanded in vitro and reprogrammed to differentiated epithelia for morphological and functional studies. We found a relatively high ({\~{}}3{\%}) ionocyte abundance in ex vivo nasal samples, with no difference between CF and control individuals. In bronchi, ionocytes instead appeared very rarely as previously reported, thus suggesting a possible proximal-distal gradient in human airways. The difference between nasal and bronchial epithelial cells was maintained in culture, which suggests an epigenetic control of ionocyte development. In the differentiation phase of the culture procedure, we used two media that resulted in a different pattern of CFTR expression: confined to ionocytes or more broadly expressed. CFTR function was similar in both conditions, thus indicating that chloride secretion equally occurs irrespective of CFTR expression pattern.
Developmental cell 2020 oct
Super-Resolution Microscopy and FIB-SEM Imaging Reveal Parental Centriole-Derived, Hybrid Cilium in Mammalian Multiciliated Cells.
Z. Liu et al.
Abstract
Motile cilia are cellular beating machines that play a critical role in mucociliary clearance, cerebrospinal fluid movement, and fertility. In the airways, hundreds of motile cilia present on the surface of a multiciliated epithelia cell beat coordinately to protect the epithelium from bacteria, viruses, and harmful particulates. During multiciliated cell differentiation, motile cilia are templated from basal bodies, each extending a basal foot-an appendage linking motile cilia together to ensure coordinated beating. Here, we demonstrate that among the many motile cilia of a multiciliated cell, a hybrid cilium with structural features of both primary and motile cilia is harbored. The hybrid cilium is conserved in mammalian multiciliated cells, originates from parental centrioles, and its cellular position is biased and dependent on ciliary beating. Furthermore, we show that the hybrid cilium emerges independently of other motile cilia and functions in regulating basal body alignment.
View All Publications